Stem Cells and Regenerative Medicine
Regenerative medicine is the process of creating living, functional tissues to repair or replace damaged cells, tissues, or organs in order to treat or cure conditions caused by aging, disease, damage, or congenital defects. Regenerative medicine may be able to prompt the body to heal itself by stimulating organs previously considered incapable of healing themselves, and it provides a potential solution to overcome the shortage of organs available for donation. A recent discovery also provides opportunities to address immune rejection of transplanted tissue, a major problem in regenerative medicine. Researchers have discovered that it is possible to reprogram adult cells to a pluripotent state, giving scientists the ability to generate differentiated cells and tissues using cells from specific patients. This will facilitate individualized medicine and eventually lead to specialized therapies.
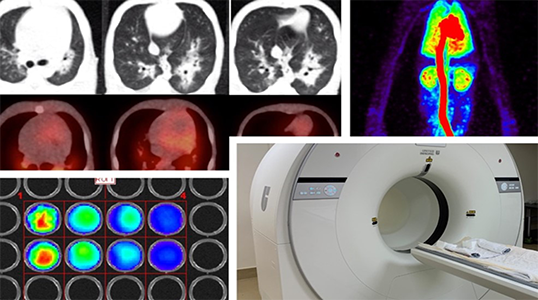
The field of regenerative medicine is moving toward translation to clinical practice and is becoming increasingly dependent on animal models to provide information about the potential therapeutic efficacy of new technologies. However, significant challenges remain, including generating the correct type and quantity of the specific cells required for replacement therapy, successfully introducing these cells into the proper environment in vivo, and overcoming immune reactions. Finding solutions to these problems will require extensive testing in experimental animal models.
Along with rodents, several other animal species are being developed as models for use in regenerative medicine. Understanding the properties and capabilities of stem cells derived from such animals as fish, rabbits, dogs, pigs, sheep, goats, and monkeys will help ensure that the most appropriate systems are used for modeling particular human diseases or for other medical applications. Non-rodent species, especially “large animal models,” provide important advantages for transplantation studies, including large size, similarity to human physiology and pathology, and longer life span, thus facilitating translation to studies in humans. The use of animal stem cells as a model for human cells in procedures related to regenerative medicine requires an in-depth understanding of common regulatory pathways, as well as species-specific properties and their impact on potential therapeutic applications.
ORIP has published several funding opportunity announcements, including PAR-16-093, PAR-16-094, and PAR-16-322 “Improvement of Animal Models for Stem Cell–Based Regenerative Medicine,” as part of its effort to respond to the needs and challenges identified in the report from the 2012 workshop “Improving Animal Models for Regenerative Medicine.” This initiative was intended to facilitate stem cell–based therapies for regenerative medicine. The current Division of Comparative Medicine efforts focus on the following areas: (1) comparative analysis of animal and human stem cells to help select the most predictive and informative model systems, (2) development of new technologies for stem cell characterization and transplantation, and (3) improvement of animal disease models for stem cell–based therapeutic applications.
Apply for funding under PAR-25-273 “Development of Animal Models and Related Biological Materials for Research (R21),” RFA-OD-22-013 “Resource-Related Research Projects for Development of Animal Models and Related Materials (R24),” and Parent R01 PA-25-301, which currently supports improvement of animal models for stem cell–based regenerative medicine
Examples of Projects Funded by ORIP:
The National Primate Research Centers
The National Primate Research Centers (NPRCs) have been at the forefront of stem cell biology and regenerative medicine research. Most NPRCs have capacities related to or specialize in stem cell biology, transplantation, and regenerative medicine research.
https://www.nprcresearch.org/Research/Page/ViewPage?id=57a61153-83b7-4b4f-935d-e34b284b04cc
National Swine Resource and Research Center
The National Swine Resource and Research Center provides infrastructure to ensure that biomedical investigators have access to critically needed swine models, including for studies of regenerative medicine products in the areas of cardiovascular, orthopedic, and wound-healing research.
U42OD011140
University of Missouri
Columbia, MO 65211
Transplantation of Testis Stem Cells in Large Animals
R01OD016575
Ina Dobrinski
University of Calgary
2500 University Dr NW
Calgary, AB T2N 1N4, Canada
Developing second generation SCID pig models: filling the gaps to improve translation of therapeutics in regenerative medicine
R24OD028748
Christopher Tuggle
Iowa State University
Ames, IA
Genetically Diverse Mouse Embryonic Stem Cells: A Platform for Cellular Systems Genetics
R24OD030037
Christopher Lee Baker, Steven Carmen Munger, Laura G. Reinholdt
The Jackson Laboratory
Bar Harbor, ME
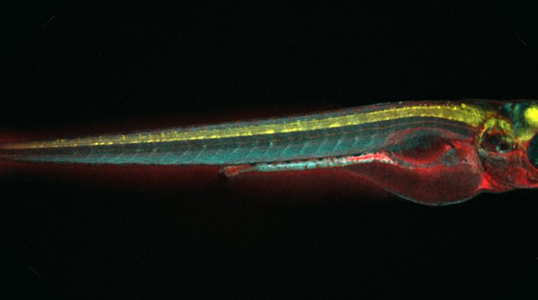
Developing preclinical xenograft models in zebrafish
R24OD031955
David Michael Langenau
Massachusetts General Hospital
Boston, MA
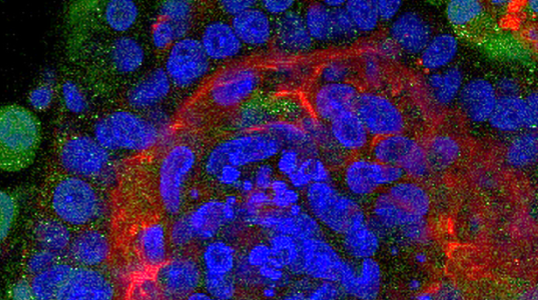
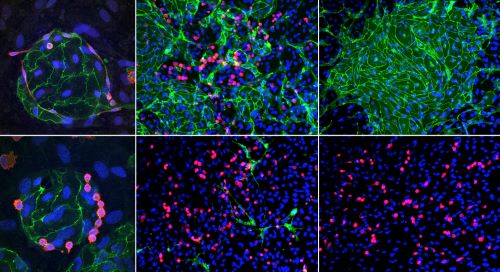
Novel hematopoietic humanized mouse model to study CAR-T therapy-associated cytokine release syndrome
R21OD034476
Yong Fan
Allegheny Health Network Research Institute
Pittsburgh, PA
A Novel Large Animal Model for Studying the Developmental Potential and Function of LGR5 Stem Cells in Vivo and in Vitro
R21OD034080
Jorge A. Piedrahita
North Carolina State University
Raleigh, NC
Novel humanized mouse model of mucosal immunity
R21OD032454
Anna Karolina Palucka
The Jackson Laboratory
Bar Harbor, ME
Developing a new chordate model for stem cell biology and regeneration
R21OD030520
Anthony W. De Tomaso
University of California, Santa Barbara
Santa Barbara, CA
Mesenchymal stem/stromal cells to enhance cytotoxic T cell immunity during HIV infection
R21OD032351
Amir Kol
University of California, Davis
Davis, CA
Direct generation of complex genetically-modified mouse models via embryonic stem cells
R21OD031973
Duancheng Wen
Weill Cornell Medicine, Cornell University
New York, NY
Genetically enabling Hydra oligactis for comparative studies in development, regeneration and aging
R21OD037741
Celina Juliano
University of California, Davis
Davis, CA
Establishment of xenopus stem cell lines
R21OD033669
Nadege Gouignard
University of Wisconsin–Milwaukee
Milwaukee, WI
Establishing Acomys as a genetic platform for regeneration research
R21OD036471
Kathleen Joyce Millen
Seattle Children's Hospital
Seattle, WA
Related Research Highlights
Recent Selected Grantee Publications
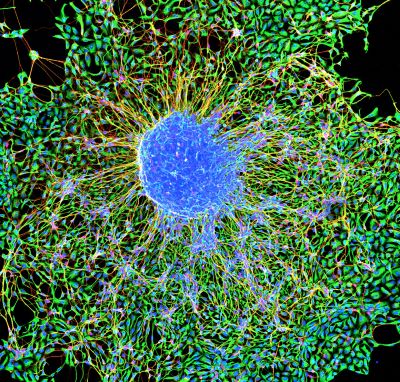
Small-Diameter Artery Grafts Engineered from Pluripotent Stem Cells Maintain 100% Patency in an Allogeneic Rhesus Macaque Model
Zhang et al., Cell Reports Medicine. 2025.
Globally, the leading cause of death is occlusive arterial disease, but surgical revascularization improves patient prognosis and reduces mortality. Vascular grafts often are needed in coronary…
Differentiation Success of Reprogrammed Cells Is Heterogeneous In Vivo and Modulated by Somatic Cell Identity Memory
Zikmund et al., Stem Cell Reports. 2025.
Nuclear reprogramming can change cellular fates, yet reprogramming efficiency is low, and the resulting cell types are often not functional. Researchers used nuclear transfer to Xenopus eggs to…
Local Tissue Response to a C-X-C Motif Chemokine Ligand 12 Therapy for Fecal Incontinence in a Rabbit Model
Ruetten et al., American Journal of Physiology—Gastrointestinal and Liver Physiology. 2025.
Obstetric anal sphincter injury (OASI) occurs in 2–7% of vaginal childbirths. Surgical interventions for OASI are suboptimal, with 30% of women reporting continued reduction in quality of life due to…