Development of Patient Avatars to Treat Human Diseases: How Two JAX Centers Are Advancing Research Through Genetic Models
Between 25 to 30 million Americans are impacted by rare diseases, but only 5% of rare diseases have treatments approved by the U.S. Food and Drug Administration (FDA), underscoring a profound need for more research in this field. For individuals and families affected by rare diseases, each day is a battle for answers, treatment, and hope. The ORIP-supported The Jackson Laboratory (JAX) Center for Precision Genetics (JCPG) prioritizes the development of precision models to study genetic diseases. The JCPG is one of three U54 centers funded under the Precision Disease Modeling Initiative. The JCPG collaborates closely with the JAX Rare Disease Translational Center (RDTC) to promote translation of gene therapies to the clinic. Both programs are bridging the gap between scientific discovery and patient-centered solutions, providing the biomedical community with advanced models needed to develop precision therapies for genetic disorders.
Dr. Cathleen Lutz, Vice President of the RDTC, focuses on developing and testing gene therapies for ultra-rare diseases because they provide a gateway to understanding other chronic diseases that have genetic bases. In 2021, the annual cost of care for people with chronic diseases in the United States was $413 billion. Nearly 80% of rare diseases have genetic origins and are classified as chronic.1 “Rare diseases aren’t as rare as people think; I think everyone knows a person or family affected by a rare genetic disease,” Dr. Lutz stated. The JCPG leverages diagnostic sequencing to identify underlying genetic causes of human diseases and to find treatments.
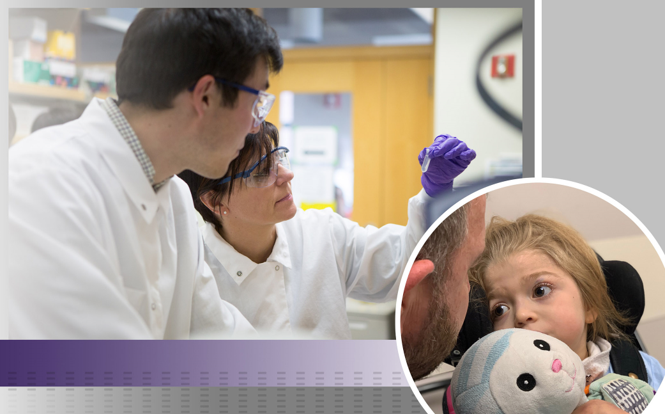
For many human diseases, the path to treatment begins with a mouse. The JCPG and RDTC work together to develop mice with altered DNA to serve as avatars (a model to study the effects of genetic diseases in patients). These models help with developing gene therapy tools that modify genomic structures to stop or reduce the progression of the disease, ensuring that only the most promising therapies move forward to patients in clinical trials. These efforts emphasize rigor and transparency to ultimately advance biomedical research for all diseases.
The JCPG’s approach to modeling human diseases starts with understanding their genetic basis so that treatments can be applied broadly to prevent a wide range of genetic diseases. A powerful example of this is the progress made on amyotrophic lateral sclerosis, a fatal disease caused by the SOD1 mutation that has been treated successfully with gene therapy. Similar breakthroughs are expected for other neurodegenerative diseases—as well as colon cancer and breast cancers—paving the way for strategies that could prevent symptoms of more common diseases before they even begin.
The research on these diseases is made possible by patients’ families and the vast network of collaborators with expertise in specific topics and models. “It’s a small community of like-minded people with the same end goal of getting the science out there and helping the patients,” noted Dr. Lutz. Her team has forged strong relationships with patient families. The power of patient advocacy is critical to shaping research priorities. JAX’s inspiration for the JCPG stemmed from the #WeNeedAMouse campaign, led by Sally Jackson and Luke Rosen on behalf of their daughter, Susannah, who was diagnosed with a neurodegenerative disease caused by a KIF1A mutation. Their movement caught Dr. Lutz’s attention, which led to the development of patient avatars for KIF1A Associated Neurological Disorder and a treatment for Susannah.
In addition to generating mouse models, the JCPG is actively using new approach methodologies (NAMs). For example, the Center engineered KIF1A patient mutations into human induced pluripotent stem cells and is differentiating these lines into motor neurons to better understand the deficits related to axonal transport. These cells will also be used to screen gene editing therapies that are currently in development. “It’s the triangulation of new technologies—human cell lines and humanized mouse models—that make for a powerful approach to tackling these diseases,” stated Dr. Lutz. By incorporating NAMs, research can move quickly and with relevance to the human genome.

The JCPG is patient centered and works closely with patients’ families to help find solutions. Families can submit nominations on the JCPG website for researchers to develop models and study their child’s disease. Parents are not only caregivers and advocates for their children: they also are the driving force behind the research, bringing attention to diseases that might otherwise go unrecognized. “Parents are our best partners,” Dr. Lutz explained, “because they are incredibly motivated and inspire us to find a cure as fast as we can.” Families often find researchers, raise funds, and push for clinical trials, ensuring that their children’s conditions are not ignored.
A notable example of this is Dr. Lutz’s team’s efforts on alternating hemiplegia of childhood (AHC), a neurological disorder that presents in children before 18 months of age (Figure 1). Inspired by two young patients, Annabel and Henry, Dr. Lutz’s team has made significant strides using AHC mouse models developed through the JCPG. Through academic collaborations, her team also is evaluating two promising gene therapy approaches for AHC, with plans to test these treatments in AHC avatars.
A recent study published in Cell by Dr. Lutz’s group and her collaborator, Dr. David Liu at the Broad Institute, demonstrated that gene editing strategies for AHC provided remarkable efficacy in cell and mouse models for AHC.2 The study began with the design and testing of editors for efficiency and accuracy in human cell lines. The study then moved to animal models to understand the therapeutic effects of these prime editing strategies. “For neurodevelopmental disorders, it is not always a given that a therapeutic can have an effect on a disease after birth. Not only did we demonstrate the benefits of a therapeutic after birth in these animals, but we did so in a neurological disorder, where delivery of therapeutics to the brain is especially challenging,” explained Dr. Lutz.

“We don’t want to take too much time and prolong the disease for the patients,” Dr. Lutz continued. This philosophy was evident in the case of Willow, a young patient with multiple sulfatase deficiency (MSD), a fatal lysosomal storage disease (Figure 2). In one of eight studies accepted into the Foundation for the National Institutes of Health Accelerating Medicines Partnerships® Bespoke Gene Therapy Consortium, the JCPG developed a gene therapy that showed promise in restoring the SUMF1 gene in MSD.3 Unfortunately, Willow passed away on October 5, 2024, before she could receive treatment. Her story, highlighted in the documentary The Zebra and the Bear, serves as a reminder of why the work at the JCPG and RDTC is critical. Willow’s mother, Ms. Amber Olsen, has kept the momentum going for many patients through her advocacy (Figure 3). Her journey illustrates a painful reality—for many children, the treatment for a genetic disease comes too late, leaving families in mourning but determined to fight for others. Dr. Lutz is inspired by parents like Amber, whom she is still in contact with, and is driven to keep pursuing the research. “Willow remains our inspiration and our hope that the next child diagnosed with MSD will receive this critical treatment.”
Patients are involved in every step of the process to develop therapies. Patients and their families participate in monthly meetings with collaborators and research teams. They learn about the therapeutics that potentially will be administered in a manner to ensure the safety and success of these therapies. Patients’ families also share their experiences at each meeting. “Those of us with children—we celebrate the firsts. A lot of times, these families mourn the lasts, such as the last time their child ate independently or was able to say ‘Mommy,’” Dr. Lutz shared. “Hearing the patients’ stories continuously motivates us to move forward with research.” Input from the parents goes beyond finding a cure and includes improving the quality of life for the patients. For example, boys and young men with Duchenne muscular dystrophy want to have enough independence to drive, to have better control when playing video games, or to shave. “Everyday activities that we take for granted mean so much to these patients,” explained Dr. Lutz. These meetings with parents give the researchers insight into where to focus their research goals.
A major goal in genetic research is to reduce the financial barriers while ensuring that the research momentum does not stall—particularly for ultra-rare genetic conditions, which receive fewer pharmaceutical investments. Another goal is to make a more efficient regulatory framework that balances safety with urgency, recognizing that for many patients and their families, time is the biggest enemy. Dr. Lutz’s team is working with the FDA and policymakers to streamline the approval process. “We must do significantly better for these kids,” stated Dr. Lutz. “Any time the research, funding, or investments stop, the burden falls back on the parents.”
Despite these hurdles, the future of genetic diseases research is brighter than ever. Dr. Lutz believes that one of the most exciting frontiers is the potential for preventive treatment of rare diseases, emphasizing the need for early genetic testing and intervention. “I think there are preventative measures through gene therapy and genome sequencing if we can get to the kids in time.” Dr. Lutz emphasized that developing a mouse model means that about 80% of the foundational work toward developing a gene therapy has already been completed.
The work being done at the JCPG through ORIP funding is leading a revolution in genetic disease solutions, giving patients and their families hope for genetic models serving as patient avatars and innovative gene therapies. “We are just getting started and will make strides in the future of genetic diseases,” declared Dr. Lutz. All mouse models developed at the JCPG are available to researchers through the Mutant Mouse Resource and Research Centers, an ORIP-funded mouse repository, which saves research time. “ORIP has always had a vision of how model organisms can help today, but also in the future … I’m incredibly grateful to ORIP for having this resource-minded approach in supporting science,” stated Dr. Lutz. Her team remains committed to its mission to ensure that every patient gets a chance at a healthier future. With the dedication of scientists, families, and advocates, a future with cures for genetic diseases is becoming a reality.
ORIP renewed the Pilot Centers for Precision Disease Modeling Initiative (PAR-24-305) by building on the success of funding for the previous program (PAR-20-085) and supported three U54 Centers (The Jackson Laboratory Center for Precision Genetics [U54OD030187], Baylor College of Medicine Center for Precision Medicine Models [U54OD030165], and The University of Alabama at Birmingham Pilot Center for Precision Animal Modeling [U54OD030167]). The new effort aimed to develop collaborative research centers with increased focus on creating pipelines for research community–nominated unique human genomic variants linked to diseases for cost-effective, high-throughput testing in such models as mice, rats, Caenorhabditis elegans, zebrafish, Drosophila, Xenopus embryos, and human induced pluripotent stem cells. By integrating advances in genomics and animal modeling, the program enhances the predictive power of preclinical research. This effort directly aligns with ORIP’s mission to develop and provide essential research infrastructure—including innovative animal models—that supports biomedical discovery and advances human health.
References
1 Rezaei F, Sanagoo A, Peyrovi H, et al. Persistent suffering: living experiences of patients with rare disease: an interpretative phenomenological study. J Educ Health Promot. 2023;12:224. doi:10.4103/jehp.jehp_1010_22.
2 Sousa AA, Terrey M, Sakai HA, et al. In vivo prime editing rescues alternating hemiplegia of childhood in mice. Cell. 2025 Jul 15:S0092-8674(25)00740-8. doi:10.1016/j.cell.2025.06.038.
3 Presa M, Bailey RM, Ray S, et al. Preclinical use of a clinically-relevant scAAV9/SUMF1 vector for the treatment of multiple sulfatase deficiency. Commun Med (Lond). 2025;5(1):29. doi:10.1038/s43856-025-00734-9.



