Profile of a Promising HIV/AIDS Scholar: Riti Sharan, Ph.D.
As an immunologist studying HIV, latent tuberculosis infection (LTBI), and possible treatments, Dr. Riti Sharan (Figure 1) has been intrigued by the human body since high school, particularly the complex and varied mechanisms by which it defends itself against pathogens.
A career in biomedical research was Dr. Sharan’s childhood dream. She earned her undergraduate degree from Bangalore University in Bengaluru, India, and a master’s degree in microbiology through the honors program at Panjab University in Chandigarh, India. On the basis of her master’s program work, which focused on understanding the virulence mechanisms of Stenotrophomonas maltophilia, she received a full scholarship from Central Queensland University (CQUniversity) in Rockhampton, Australia, to pursue a Ph.D. Remarkably, Dr. Sharan completed her doctorate in 3 years, authored and co-authored five peer-reviewed publications, and was in the top 2% of Ph.D. candidates at CQUniversity. Dr. Sharan credits one of her mentors, Dr. Robert H. Reed, who was Pro-Vice-Chancellor of Learning and Teaching at CQUniversity at the time, with inspiring her achievements, noting that he “cared more about everything—not just the science, but the overall understanding of the subject, especially in terms of ethics and compliance.”
During her doctoral training, Dr. Sharan’s research interest in host–pathogen (bacteria) interactions led her to develop a mouse model to evaluate the effects of bacterial infections. She used this mouse model to study the effectiveness of copper as an antibacterial agent. To this end, she demonstrated for the first time that copper stress decreases the infectivity of Salmonella enterica serovar Typhimurium in normal mice.1 Subsequently, she developed a cost-effective technique using copper storage vessels to reduce the incidence of waterborne diseases in developing nations.
Dr. Sharan’s research interest expanded from studying bacteria and host pathogens to investigating the human body’s immune responses to bacteria. Because tuberculosis (TB), which is caused by Mycobacterium tuberculosis (Mtb), was endemic in India,2 she reoriented her efforts to address this health problem affecting the population in her country of origin. She completed a 1-year postdoctoral fellowship focused on TB at the United Nations International Centre for Genetic Engineering and Biotechnology and continued her postdoctoral studies in immunology at the Pasteur Institute in Lille, France. Under the mentorship of her team leaders at the Pasteur Institute, Dr. Sharan made a pioneering discovery identifying interleukin-22 as a therapeutic target to treat chronic obstructive pulmonary disorder exacerbation by non-typeable Haemophilus influenzae and Streptococcus pneumoniae in a mouse model of cigarette smoking.3
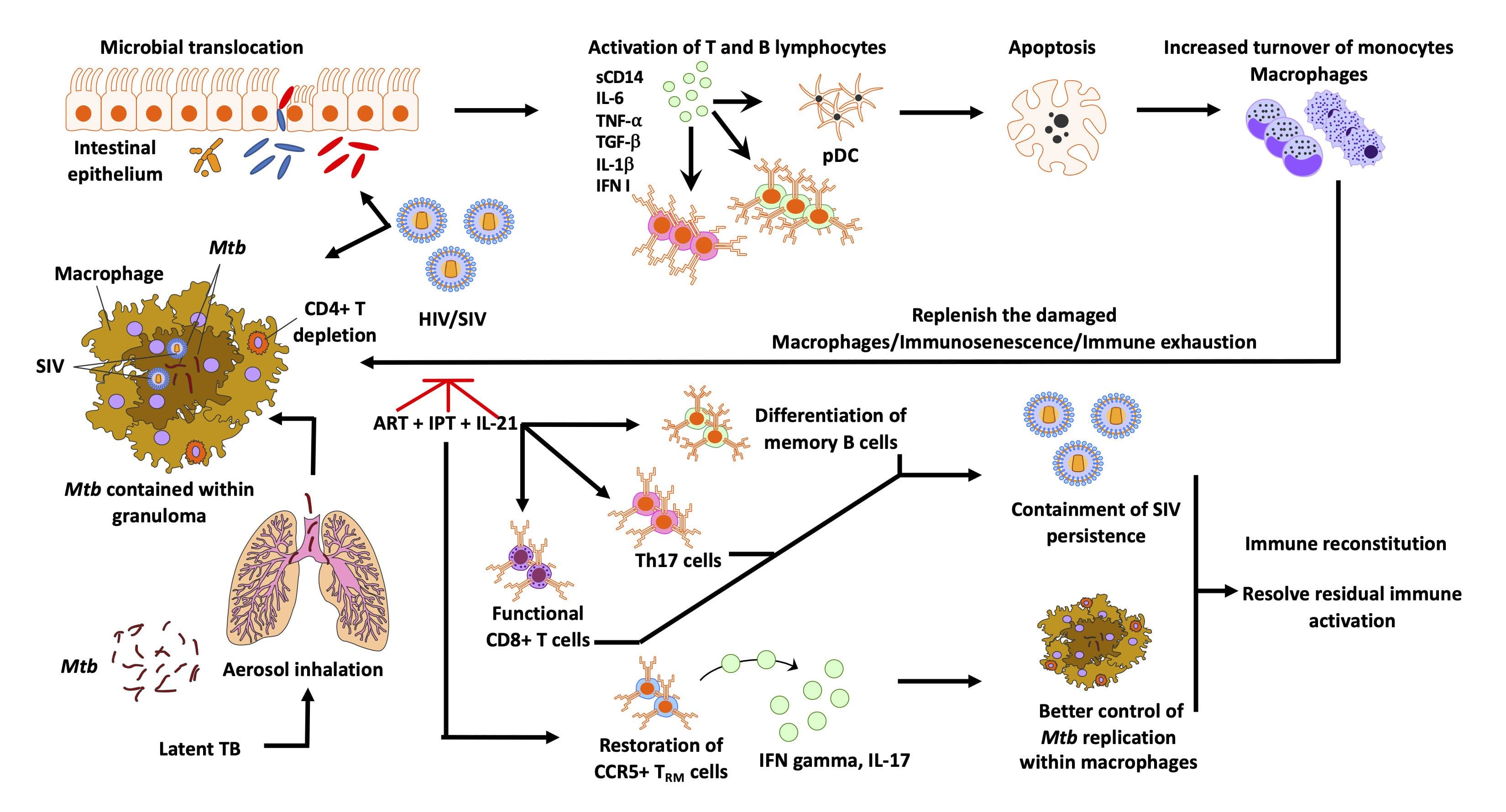
Dr. Sharan continued her postdoctoral studies in the United States under the direction of the National Institutes of Health (NIH)-supported principal investigator Dr. Jeffrey Cirillo, Director, Center for Airborne Pathogen Research and Imaging at the Texas A&M University Health Science Center. She combined her immunology and respiratory backgrounds to test TB vaccine candidates and perform in vivo imaging in mouse and guinea pig models. With her extensive training in preclinical small-animal models and respiratory pathogens, she advanced to a staff scientist position investigating the TB/HIV co-pandemic using an established nonhuman primate (NHP) model of TB.4 Dr. Sharan’s project focused on evaluating the effect of early antiretroviral therapy (ART) in TB/simian immunodeficiency virus (SIV) coinfection in Mtb-infected macaques. This research formed the basis for her NIH K01 application (Figure 2).
In 2020, Dr. Sharan received an HIV/AIDS Scholars Program K01 award to study the impact of HIV in reactivating LTBI, to which worse outcomes in individuals with HIV or AIDS have been attributed. NIH’s Office of Research Infrastructure Programs (ORIP) and Office of AIDS Research (OAR) launched the HIV/AIDS Scholars Program in 2016 to support early-stage investigators (ESIs) in research and training. A signature feature of this program is the mentored career development. A mentoring team composed of at least a primary mentor and a co-mentor who are active in HIV/AIDS preclinical/clinical research supervises the career development and research experience of the K01 Scholar. With this program, ORIP aims to facilitate the development of effective HIV/AIDS treatment and prevention strategies and has increased the workforce that can use NHPs as preclinical models.
The overarching goal of Dr. Sharan’s K01 project was to identify the key correlates of SIV-mediated chronic immune activation before, during, and after ART to develop therapeutic interventions adjunct to ART in coinfected humans. This ORIP/OAR project aligns with the NIH HIV/AIDS research priority to address HIV-associated comorbidities and coinfections. Dr. Sharan’s study was the first to examine the impact of the timing of combination ART on LTBI reactivation in a biologically and physiologically relevant NHP model. Her key finding was that initiating ART early significantly reduces macrophage turnover and chronic immune activation in Mtb/SIV coinfected rhesus macaques.5 In her most recent research that builds on these efforts, she reported that isoniazid and rifapentine treatment effectively reduces persistent Mtb infection in macaque lungs.6
During her K01 experience, Dr. Sharan received intensive research career development under the guidance of an experienced mentorship team composed of established researchers at Southwest, Emory, Tulane, and Yerkes National Primate Research Centers—which are part of the National Primate Research Centers Consortium supported by ORIP—and Washington University in St. Louis. The K01 support also allowed Dr. Sharan to attend scientific conferences and workshops to meet and network with peers. She remarked that “more than 15 ESIs have reached out over the years to ask for research updates and advice on securing a K01 award.” Dr. Sharan credits the K01 award from ORIP/OAR with advancing her career trajectory from “medium speed” to “full throttle.”
Dr. Sharan’s success and career development, greatly facilitated by her K01 award, speak to her resilience in this field. As her father always taught her, “Never give up, smash stereotypes, and be your own hero. Believe in yourself and do what’s right.” She continues to follow these principles. Beyond the ORIP/OAR K01, Dr. Sharan is striving to become an independent NIH-funded researcher with her own laboratory. With the help of her mentors, she submitted her first R01 application and received her first NIH R21 grant in August 2022, funded by the National Institute of Allergy and Infectious Diseases. Her project is titled “Single-Cell Transcriptomics to Identify LTBI Reactivation Markers in TB/HIV Co-infection.” She also is a core scientist at the Southwest National Primate Research Center and has applied for faculty positions, with the goal of conducting translational and foundational research and making a difference in TB and HIV.
For additional information on the HIV/AIDS Scholars Program, visit orip.nih.gov/comparative-medicine/programs/training-and-career-development/individual-training-grants.
References
1 Sharan R, Chhibber S, Reed RH. A murine model to study the antibacterial effect of copper on infectivity of Salmonella enterica serovar Typhimurium. Int J Environ Res Public Health. 2011;8(1):21–36. doi:10.3390/ijerph8010021.
2 Spertini F, Audran R, Chakour R, et al. Safety of human immunisation with a live-attenuated Mycobacterium tuberculosis vaccine: a randomised, double-blind, controlled phase I trial. Lancet Respir Med. 2015;3(12):953–962. doi:10.1016/S2213-2600(15)00435-X.
3 Sharan, R, Perez-Cruz, M, Kervoaze G, et al. Interleukin-22 protects against non-typeable Haemophilus influenzae infection: alteration during chronic obstructive pulmonary disease. Mucosal Immunol. 2017;10:139–149. doi:10.1038/mi.2016.40.
4 Kaushal D, Mehra S, Didier PJ, Lackner AA. The nonhuman primate model of tuberculosis. J Med Primatol. 2012;41(3):191–201. doi:10.1111/j.1600-0684.2012.00536.x.
5 Sharan R, Ganatra SR, Bucsan AN, et al. Antiretroviral therapy timing impacts latent tuberculosis infection reactivation in a Mycobacterium tuberculosis/SIV coinfection model. J Clin Invest. 2022;132(3):e153090. doi:10.1172/JCI153090.
6 Sharan R, Ganatra SR, Singh DK, et al. Isoniazid and rifapentine treatment effectively reduces persistent M. tuberculosis infection in macaque lungs. J Clin Invest. 2022;e161564. doi:10.1172/JCI161564.



