Mutant Mouse Resource & Research Centers Develop New Mouse Models for COVID-19 Research
Animal models are critical for advancing our understanding of the infectivity, pathogenesis, and complications of infectious diseases. The importance of model organisms was highlighted when COVID-19 began spreading around the world a few years ago. Several mouse models had been established to study coronavirus infectivity and pathogenesis; at the onset of the pandemic, however, few models existed to investigate the novel SARS-CoV-2 virus (Figure 1). Supported by ORIP, the Mutant Mouse Resource & Research Centers (MMRRCs) began developing new models for COVID-19 research—mice that express human proteins known to be involved directly with virus binding, entry, and activation in mammalian cells. “These humanized models are going to be great for studying not only pathophysiology and for looking at immunologic and inflammatory response, but also for drug targeting, drug responsiveness, and, of course, for vaccines,” explained Dr. Kevin C. Kent Lloyd, Distinguished Professor of Surgery at the University of California, Davis (UC Davis) School of Medicine and Project Director for the MMRRC at UC Davis.
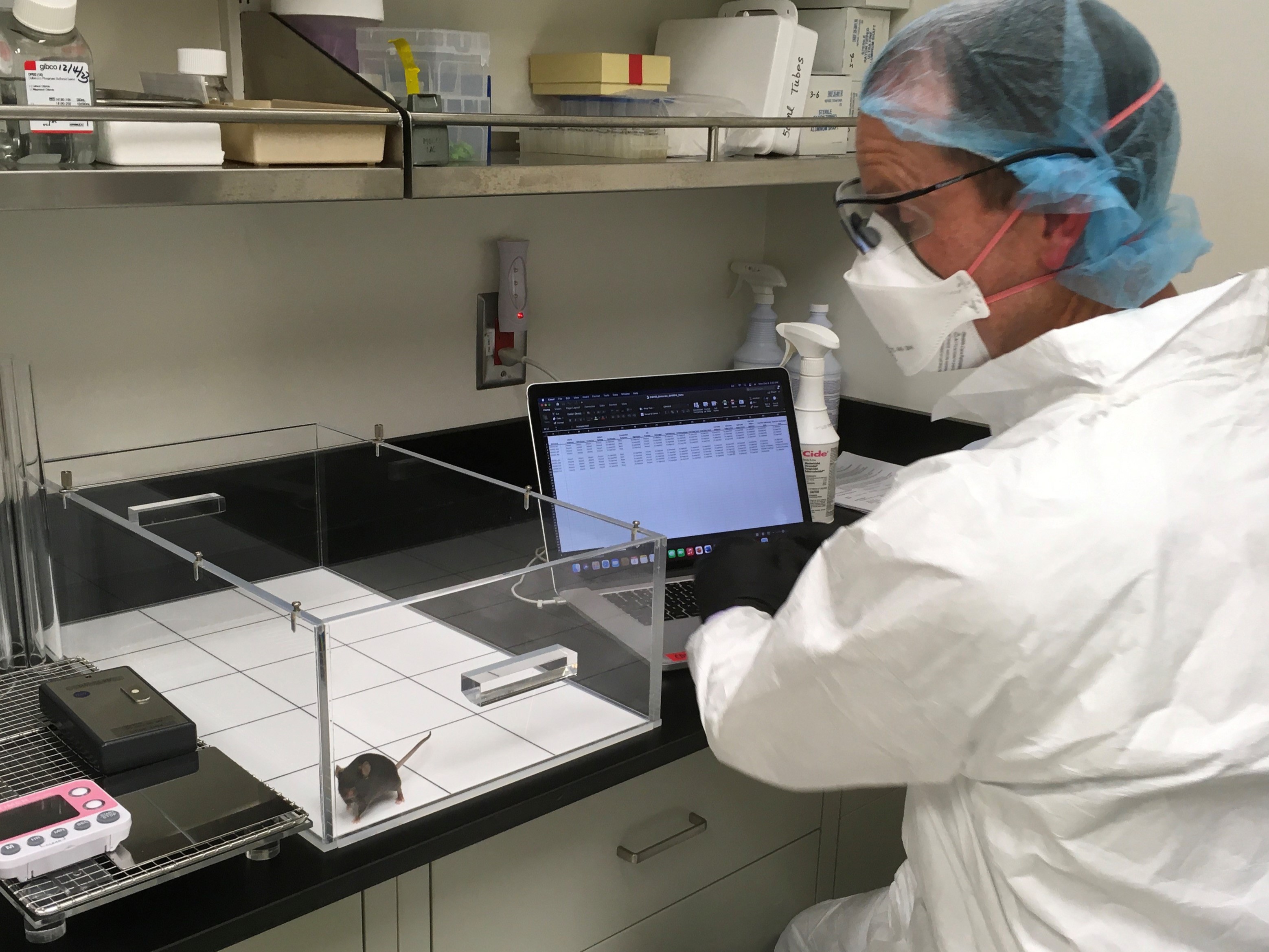
The MMRRC at UC Davis is part of a consortium of academic and private institutions that together host repositories of mutant mice that are available to researchers around the world. In addition to the location at UC Davis, MMRRC archive and distribution facilities have been established and continuously funded at The University of North Carolina at Chapel Hill (UNC), the University of Missouri (MU), and The Jackson Laboratory (JAX). An Informatics, Coordination and Service Center housed within the UC Davis Mouse Biology Program provides centralized data coordination, processing, and infrastructure that enable the MMRRC facilities to function as a single entity. Funding from ORIP supports donor deposition and maintenance activities; mouse distribution is funded by requesting investigators via service fees. The MMRRCs offer assorted services, including assisted reproduction, colony management and breeding, genetic analysis, pathology and diagnostics, and various forms of phenotyping (e.g., behavioral, metabolic, microbiome) (Figure 2).
Mouse Models for SARS Infection
Because of their role in the maintenance, distribution, and analysis of mouse models for basic and preclinical research, the MMRRC repositories were critical during the COVID-19 pandemic. Mouse models for studying coronavirus infections had been established but were not entirely suitable for research related to COVID-19. To fill this gap, MMRRC team members worked quickly to establish new mouse lines to aid in developing vaccines and therapeutic drugs to use in the fight against SARS-CoV-2.
In 2003, long before the COVID-19 pandemic, a novel respiratory illness had emerged globally, with thousands of cases recorded in China and Hong Kong and hundreds of cases reported in Canada, Singapore, and Taiwan. The new disease was named severe acute respiratory syndrome (SARS) and was caused by a coronavirus that was later named SARS-CoV-1. Researchers attempting to study SARS realized that wild-type mice were resistant to infection.1 SARS infections are mediated by viral spike (S) glycoproteins binding to angiotensin-converting enzyme 2 (ACE2) receptors expressed on the human host cell membrane. However, unlike in humans, the mouse ACE2 receptor (mACE2) binds to the SARS-CoV-1 S glycoprotein with very low affinity, removing the gateway to viral invasion and infection.2 To circumvent this challenge, the transgenic K18-hACE2 mouse strain—which expresses the human form of the ACE2 (hACE2) gene under regulation of the human keratin 18 (K18) promoter—was developed. In these animals, the hACE2 protein is present on the surface of epithelial cells, and subsequently, the mice experience lethal infection when challenged with the SARS coronavirus.3
When COVID-19 emerged as a global pandemic, the K18-hACE2 mouse strain again served as a valuable resource. Upon infection with the SARS-CoV-2 virus, K18-hACE2 mice recapitulate symptoms of COVID-19 infection, including inflammation in the lungs and brain.4 Infected mice have difficulty breathing, lose weight, and die within days. Dr. Cathleen Lutz is the Vice President of the Rare Disease Translational Center and Principal Investigator of the MMRRC at JAX, a biomedical organization that conducts research in various areas and delivers mice to laboratories across the nation. Dr. Lutz described the scramble to acquire the K18-hACE2 strain in the early days of the pandemic: “We took that mouse model and brought it in, and we did a rapid expansion. We used so much of the MMRRC knowledge of rapid expansions and in vitro fertilization to get the model up and running.”
MMRRCs Develop Humanized Mouse Models
Unfortunately, using the K18-hACE2 mouse strain for COVID-19 research has several disadvantages. First, because of the method used to generate the transgenic K18-hACE2 strain, these mice harbor multiple copies of the K18-hACE2 transgene. While overexpression of the transgene enables coronavirus infections, hACE2 is not expressed at the same physiological levels or in the same tissues as in humans. K18-hACE2 mice can be used for pharmacological studies of infection (e.g., antibody testing, vaccine testing), but mouse models used to investigate the precise physiology of infection must mimic the native environment more closely. Second, transgenes like the K18-hACE2 cassette are randomly inserted into the genome and can interfere with the expression and regulation of other genes involved in infection, resulting in confounding study results. Last, because infection with SARS-CoV-2 is lethal in K18-hACE2 mice, the study of post-acute infection sequelae (commonly known as long COVID) in this model is impossible.
Supported by NIH funding, MMRRC team members at UC Davis and UNC worked quickly to create and characterize new mouse strains to serve as better models for COVID-19 research. CRISPR gene editing technology was used to replace the mACE2 gene with a single copy of hACE2, creating a humanized ACE2 knock-in mouse capable of mimicking COVID-19 infection in people. When infected with SARS-CoV-2, hACE2 knock-in mice recapitulate COVID-19 symptoms observed in human patients, including inflammation in the upper respiratory tract, altered cardiac function, and pneumonia.5 Unlike K18-hACE2 mice, these mice recover from the infection, enabling observations beyond the resolution of the infection, such as those associated with long COVID.
The MMRRC group at UC Davis has used the same techniques to create mice expressing humanized versions of other genes involved in COVID-19, including transmembrane serine protease 2 (TMPRSS2) and the FES Upstream Region (FURIN), which are both involved in viral entry into the cell following ACE2 binding. Cohorts of the triple-humanized line (i.e., ACE2/TMPRSS2/FURIN knock-in mice) have been generated and are being evaluated as a mouse model for studying SARS-CoV-2 infection and associated conditions. “Our feelings are that the double and, eventually, the triple knock-in are going to be the standard model for being able to do COVID-19 research and understanding the pathophysiology of and immunological responses to infection,” explained Dr. Lloyd.
All mouse lines have been deposited into the MMRRC. “If there’s another coronavirus outbreak or another disease process where ACE2 is particularly important, then these mice will be available ahead of time,” noted Dr. Mark Heise, a Professor of Genetics at UNC who is collaborating with the MMRRC to study the new mouse models. “I think that’s the real advantage we gained. Just like the K18-hACE2 mice were available before the pandemic, we now have more tools ready to go to help us respond to the next outbreak.” Dr. Heise highlighted UNC’s expertise in complex mouse genetics and experience with coronaviruses, which provided a solid foundation for MMRRC efforts to develop and evaluate the new mouse models in real time as the pandemic evolved.
Applications for Mouse Models: COVID-19 Infection and Beyond
The established K18-hACE2 and newer humanized mouse models have been used to study multiple aspects of SARS-CoV-2 infection. For example, human patients with certain comorbidities are more likely to exhibit poor outcomes upon infection with SARS-CoV-2. Such comorbidities, which affect the inflammatory and immune responses in patients, are being replicated and studied in the humanized mouse models. Human genetic variation also plays a role in the differences observed during SARS-CoV-2 infections.6 Dipeptidyl peptidase-4 (DPP4) is a gene that encodes a transmembrane glycoprotein involved in glucose and insulin metabolism and immune regulation. Genetic variation in the DPP4 gene is suspected to play a role in SARS-CoV-2 infection and regulate the severity of COVID‑19 disease in diabetic patients.7 The MMRRC team has generated a humanized DPP4 mouse to evaluate this connection further.
Researchers within the MMRRC network are incorporating the new mouse models into their research areas. For example, the MU hub of the MMRRC specializes in studying the role of gut microbiota in human health and disease. Because of its history as a rodent diagnostic laboratory, the MMRRC at MU is equipped to perform extensive mouse phenotyping in the areas of immunology and infectious diseases. These capabilities include the characterization of gut microbial communities and the rederivation of strains to generate mice with custom microbiomes at the MU Metagenomics Center, as well as ABSL-3 facilities available at the MU Laboratory for Infectious Disease Research (LIDR), one of 12 NIH-funded regional biocontainment facilities in the country.
“When the pandemic started,” stated Dr. Rachel Olson, chief scientific officer of the LIDR, “I was ideally placed to pivot to coordinate and make all these COVID projects happen.” Dr. Olson is collaborating with Dr. James Amos-Landgraf and Dr. Craig Franklin, Co-Directors of the MMRRC at MU, to investigate how different microbiomes or exposure to prior infections affect outcomes associated with COVID-19 infection. The LIDR facilities can also support specialized experiments, including custom aerosol exposure services and long-term studies under ABSL-3 conditions. “A big aspect is what happens after infection. How do people recover?” explained Dr. Amos-Landgraf. “We can study the impact of SARS-CoV-2 persistence and why it is persisting,” added Dr. Franklin. “We can assess long COVID in mice.”
Conclusion and Future Directions
The humanized mouse models demonstrate that the MMRRCs can quickly coordinate the development of novel strategies for in vivo analysis of new and emerging pathogens. These models will enable a more thorough understanding of SARS-CoV-2 infection and post-acute infection sequelae and will support preclinical studies of therapeutic strategies for COVID-19 and long COVID. The MMRRC directors stressed the importance of NIH and ORIP support for such critical projects. “We probably wouldn’t have been able to do this work without that support,” emphasized Dr. Heise. “It gave us the freedom to carefully design the knock-in genes—to do this in a way that would give us the best chance to recapitulate key aspects of gene regulation and expression that we’re seeing in humans.” Dr. Amos-Landgraf agreed: “The NIH supplements were crucial. I don’t think we would have ever entered the foray without them.”
Future directions for the MMRRC will involve validating and improving the existing models and coordinating activities for testing SARS-CoV-2 and other priority pathogens. “The MMRRC plays an essential role in that it is there to serve the nation—and, in fact, the world—in providing support for the use of mouse models for studying human diseases. We aim to grow and evolve to serve what’s needed in the community at the time and anticipate future needs,” Dr. Lloyd commented. “To me, we’ve only scratched the surface, especially in this era of CRISPR and genetics, in what we’re technically capable of doing.”
Please visit ORIP’s website for more information about the MMRRC program.
References
1 Zhou P, Yang XL, Wang XG, et al. A pneumonia outbreak associated with a new coronavirus of probable bat origin. Nature. 2020;579(7798):270–273. doi:10.1038/s41586-020-2012-7.
2 Martina B, Haagmans B, Kuiken T, et al. SARS virus infection of cats and ferrets. Nature. 2003;425(6961):915. doi:10.1038/425915a.
3 McCray PB Jr, Pewe L, Wohlford-Lenane C, et al. Lethal infection of K18-hACE2 mice infected with severe acute respiratory syndrome coronavirus. J Virol. 2007;81(2):813–821. doi:10.1128/JVI.02012-06.
4 Winkler ES, Bailey AL, Kafai NM, et al. SARS-CoV-2 infection of human ACE2-transgenic mice causes severe lung inflammation and impaired function. Nat Immunol. 2020;21(11):1327–1335. doi:10.1038/s41590-020-0778-2.
5 Winkler ES, Chen RE, Alam F, et al. SARS-CoV-2 causes lung infection without severe disease in human ACE2 knock-in mice. J Virol. 2022;96(1):e0151121. doi:10.1128/JVI.01511‑21.
6 Redin C, Thorball CW, Fellay J. Host genomics of SARS-CoV-2 infection. Eur J Hum Genet. 2022;30(8):908–914. doi:10.1038/s41431-022-01136-4.
7 Lim S, Bae JH, Kwon HS, et al. COVID-19 and diabetes mellitus: from pathophysiology to clinical management. Nat Rev Endocrinol. 2021;17(1):11–30. doi:10.1038/s41574-020-00435‑4.



