Precision Health and Personal Omics
Implementation of precision health has the potential to revolutionize the current paradigm of modern medicine, which is still predominantly focused on disease treatment. The idea of a proactive approach to help individuals maintain personal health and predict and prevent disease onset has become the basic premise of precision health.1 The concept of precision health originated from the jet engine industry: to prevent engine failures, avoid costly repairs, and reduce operating costs, monitoring systems with hundreds of sensors are used to collect information about the performance of the engines and the aircraft, and relay that to pilots or ground stations, which are monitored by engine manufacturers.1,2 Precision medicine also utilizes sensors ― health- and activity-monitoring devices that collect and display real-time medically relevant information. What information should be gathered and what types of technologies should be applied in the future to measure and evaluate trends in personal health data over time to make preventative health care decisions and recommendations for interventions? Precision medicine will likely benefit from combined personal “omics” data, integrating information from different technological fields, in particular, genomics, transcriptomics, proteomics, and metabolomics.3 Modern high-throughput technologies, such as high-throughput sequencing and mass spectrometry, enable the monitoring of more than 100,000 molecules simultaneously in the human body. These technologies generate large amounts of complex biochemical and biological data, which have to be processed with the use of methods of computational biology and bioinformatics.
The medical community got a glimpse into the future of personalized health monitoring and medicine several years ago, when Dr. Michael Snyder, Professor and Chair of the Department of Genetics at Stanford University School of Medicine and his collaborators, demonstrated the value of applying an integrative Personal Omics Profile (iPOP) to monitor an individual over a period of 14 months during periods of good health and disease (two viral infections4). The detailed iPOP analysis, combining metabolomic, proteomic, transcriptomic, genomic, and autoantibody data, provided medically significant molecular and physiological information to assess health risks. Knowing the specific risks, the individual had an opportunity to modify his diet and lifestyle to avert medical problems that would otherwise have ensued if the health risks had gone undiagnosed.
Recent advances in omics technologies can greatly improve our understanding of phenotypes of human diseases. In 2018, Dr. Snyder and his collaborators published the results of two studies using omics strategies to reveal perturbations associated with two conditions characterized by high morbidity (weight gain5), and high mortality (abdominal aortic aneurysm, a prevalent cardiovascular disease with a strong genetic component6). In the weight gain study5, Dr. Snyder and collaborators followed a group of 23 volunteers during periods of small weight gain and subsequent weight loss. Millions of measurements of blood and microbiomes taken over the course of the study revealed a large number of changes in gene- and molecular signatures. During the period of weight gain, transcriptomic profiling revealed that 318 genes were differently expressed between baseline and peak weight, including an increase in expression of many genes associated with lipid metabolism, inflammation, and dilated cardiomyopathy. Compared with observations at peak weight, 213 genes were expressed differently after weight loss. Many of the observed disturbances, such as lipid metabolism- and inflammation-related pathway perturbations and metabolic changes detected during weight gain, reversed after the weight dropped back to baseline levels, suggesting that negative effects of short-term weight gain can potentially be remedied. In the second study6, Dr. Snyder and his colleagues from Stanford University of Medicine integrated personal genomic and electronic health records data into an analytical framework called HEAL (hierarchical estimate from agnostic learning). Using this approach, an individual’s risks associated with abdominal aortic aneurysm can be predicted at a level comparable with many existing clinical screening tests. The effectiveness of adjusting a person’s lifestyle based on their individual genome also can be evaluated. The proposed approach can be extended for application to any complex genetic disease.
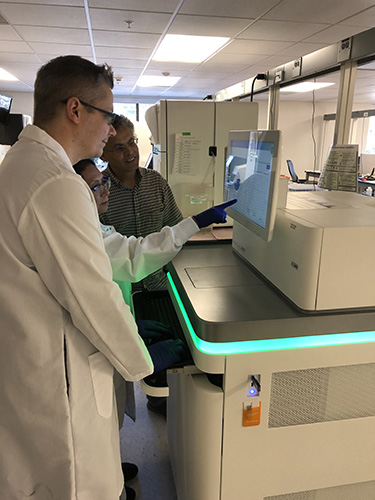
Dr. Snyder is the Principal Investigator on two S10 instrumentation grants awarded by ORIP in 2015 (S10OD025212) and 2018 (S10OD025212) to Stanford University. The grants supported acquisition of high-throughput sequencing instruments for multi-scale genomic studies for the Stanford Center for Genomics and Personalized Medicine (SCGPM) Genome Sequencing Service Center (GSSC). GSSC has an experienced staff that has been serving the sequencing needs of the Stanford community since 2009. The 2018 S10 grant supported the purchase of a NovaSeq 6000 DNA sequencing system manufactured by Illumina, an ultra-high-throughput, low-cost platform, streamlined to increase work efficiency. The NovaSeq Xp workflow allows for individual lane loading, which is ideal for GSSC, servicing the sequencing needs of a large group of users. Benefits of the NovaSeq Xp workflow include the ability of separating projects or methods by lane, multiplexing within a lane to maximize the total number of samples per flow cell, and reducing the DNA input required. Increased speed and reduced costs of ultra-high-throughput sequencing will allow large-scale genomic studies and render personal genome sequencing feasible to be used in Precision Health.7
References
1Gambhir SS, et al. Toward achieving precision health. Science Translational Medicine 2018;10(430).
2Goglia J. Aircraft Engine Monitoring: How It Works And How It Could Help Malaysia Air 370 Crash Investigators. 2014 [cited 2018 May 4]; Available from: https://www.forbes.com/sites/johngoglia/2014/03/13/aircraft-engine-monitoring-how-it-works-and-how-it-could-help-malaysia-air-370-crash-investigtors/#31c67bfd7620.
3Chen R and M Snyder. Promise of personalized omics to precision medicine. Wiley Interdisciplinary Reviews: Systems Biology and Medicine 2013;5(1):73-82.
4Chen R, et al. Personal omics profiling reveals dynamic molecular and medical phenotypes. Cell 2012;148(6):1293-307.
5Piening BD, et al. Integrative personal omics profiles during periods of weight gain and loss. Cell Systems 2018;6(2):157-170 e8.
6Li J, et al. Decoding the genomics of abdominal aortic aneurysm. Cell 2018;174(6):1361-1372 e10.
7Reuter JA, DV Spacek, and MP Snyder. High-throughput sequencing technologies. Molecular Cell 2015;58(4):586-97.



