Baylor College of Medicine U54 Program Seeks to End the Diagnostic Odyssey for Patients with Rare Diseases
With the introduction of new techniques in molecular biology—such as clinical exome sequencing, whole-genome sequencing, RNA sequencing, and metabolomics—researchers are equipped with more tools than ever to understand the genetic basis of diseases that affect human health. This ongoing discovery of novel disease genes has paved the way for structural, functional, and mechanistic insights, facilitating personalized approaches to disease management. Yet many patients, particularly those with rare diseases, wait years for a diagnosis—a phenomenon that is often referred to as the “diagnostic odyssey.” Furthermore, most known rare diseases lack a U.S. Food and Drug Administration–approved treatment.

The Center for Precision Medicine Models (CPMM) at the Baylor College of Medicine (BCM) strives to bridge this knowledge gap by developing animal models that can be used to better diagnose patients with genetic and rare diseases and develop new therapies (Figure 1). Established in 2020 with funding from ORIP (U54OD030165), the CPMM brings together expertise and resources in medical genetics, rare disease gene discovery, animal modeling, and bioinformatics. The CPMM is directed by Dr. Jason Heaney, Associate Professor, Molecular and Human Genetics, BCM, and is co-directed by Dr. Lindsay Burrage, Associate Professor, BCM, and Dr. Aleksandar Milosavljevic, Henry and Emma Meyer Chair in Molecular Genetics, BCM.
ORIP currently supports three U54 Pilot Centers for Precision Disease Modeling. These Centers enable collaborative research projects that link current personalized medicine efforts in human subjects with advances in animal genomics and technologies for genetic manipulation and creation of interspecies somatic hybrids. Data generated at the Centers are made publicly available to the research community, and NIH-funded investigators can access the resources at no cost. The CPMM focuses primarily on generating and phenotyping precision fly and mouse models for human disease.
According to Dr. Heaney, the CPMM provides critical infrastructure and resources to explore the genetic basis of diseases that have been identified in patients. “I think that’s where our strengths lie. A clinician might be interested in human genetics and say, ‘I have a patient with this genetic variation, but I don’t have a way to experimentally prove that connection,’” Dr. Heaney explained. “And that’s where we step in—to help those clinicians that don’t have funding or resources to do that work. We can come in and collaborate with them to fill in that knowledge gap.”
The CPMM team is highly collaborative, working with other research groups both within BCM and at other institutions. The CPMM centralizes resources in animal modeling, leveraging BCM’s highly prestigious programs and global expertise in the areas of human clinical genetics, human research genetics, and bioinformatics. “It takes a village to do this type of work,” Dr. Heaney stated. “To do it right, you have to have a collection of individuals with a breadth of different expertise. And we are fortunate that we have that, all right here under one institute.” BCM maintains core facilities to provide various services, including imaging, behavior, neurological function, and bone assessment. BCM is also home to one of the largest academic mouse colonies in the United States, which facilitates access to animals for model development.
Researchers use animal models to validate or confirm the causes of diseases in humans. The models also can be used to develop and test treatments for those diseases. A variety of animal models—including invertebrate organisms (e.g., worms, flies), aquatic species (e.g., zebrafish, salamanders, frogs), rodents (e.g., mice, rats), and large animals (e.g., pigs, nonhuman primates)—commonly are used in biomedical research. Dr. Heaney explained that fruit flies and mice—the CPMM’s primary models—offer unique, complementary advantages for biomedical research. The fly, which has a short life span and rapid reproduction life cycle, is often well-suited for studies of genetic mechanism. The mouse, which is more genetically similar to humans, can be used for validating a specific human disease phenotype that would not be present in flies (e.g., heart or skeletal defects).
The CPMM accepts nominations from clinicians, genetic counselors, and researchers who are interested in further exploring potentially disease-causing genetic variants using animal models. The CPMM is disease agnostic, meaning that nominations are not restricted to a particular biological question or system—although rare diseases are an area of particular interest. All nominations are reviewed by a selection committee and are evaluated based upon a broad set of criteria, including suitability for modeling by the CPMM, novelty of the variant and potential impact, quality and completeness of information in the nomination, and willingness of the applicant to communicate and collaboratively engage with the team.
To date, the CPMM has received 105 nominations, of which 46 were accepted. The accepted nominations are being studied at the CPMM using the appropriate model (i.e., flies, mice, or cell lines). The nominations have helped enable successful research outcomes that offer new insight into diseases. These studies are relevant to various NIH institutes, centers, and offices and span numerous research institutions across the United States. Research topics have included neurodevelopmental disorders,1-3 limb malformations,4 and infectious diseases.5 Researchers also have published papers highlighting the utility of novel genetic tools and technologies.6–8
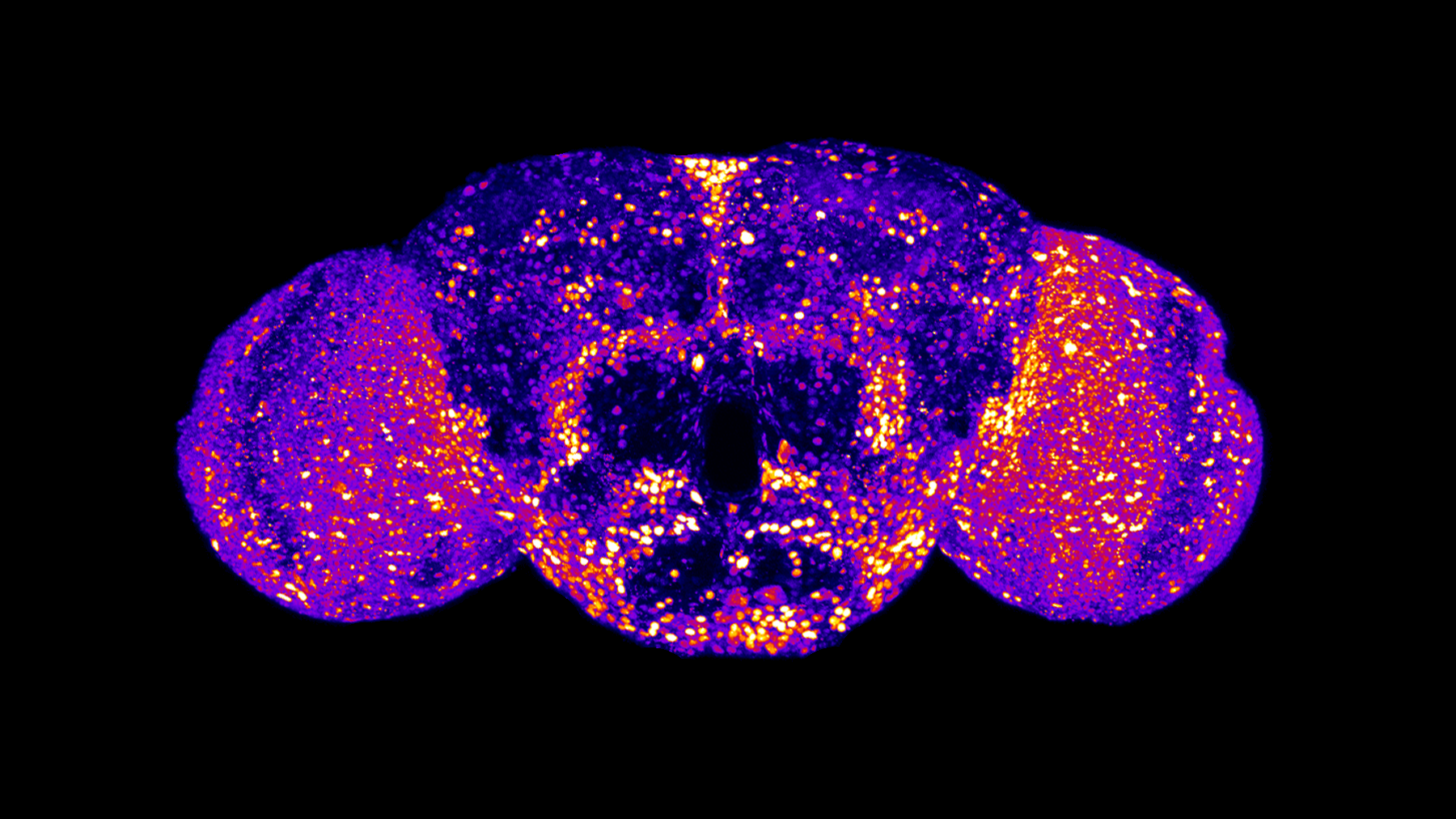
The CPMM has supported researchers in studying how variants in the UBA5 gene (Figure 2) contribute to developmental and epileptic encephalopathy (DEE), a group of disorders that cause seizures and developmental delays in children. Dr. Hugo Bellen, Distinguished Service Professor, Molecular and Human Genetics, and Dr. Shinya Yamamoto (both are co-leads of two CPMM Sections at BCM) in collaboration with the Jan and Dan Duncan Neurological Research Institute at Texas Children’s Hospital, recently developed humanized fruit fly models to characterize the phenotypes (both in vivo and in vitro) associated with different UBA5 gene variants.1
The team reported a broad spectrum of affected phenotypes in the fly models, including viability, developmental timing, life span, locomotor activity, and bang sensitivity, as well as functional effects (e.g., protein stability, ATP binding, protein activation, protein transthiolation). The team’s findings provide a foundation for further studies on DEE and could lead to new treatment options for patients. The CPMM is now developing mouse models for UBA5 variants to provide a preclinical tool to probe for new DEE therapies. “I think this project really highlights the value of our Center and full breadth of the story,” Dr. Heaney reflected. “We have shown the power of what the fly model can achieve, and we are shifting into a different system to show the power of what the mouse model can achieve as a platform for therapeutic studies.”
The CPMM worked in partnership with the Raiden Science Foundation, which is overcoming traditional research barriers to advance treatment for UBA5 disorder. Mr. Tommy Pham, Co-founder and President of the Raiden Science Foundation, explained that the fly models created by Dr. Bellen’s team led to the discovery of key genetic variants associated with the disease severity. Pham’s son, named Raiden, is affected by UBA5 disorder. These animal models present avenues for testing new therapies, offering hope for Raiden and other families in the UBA5 disorder community. Mr. Pham spoke on the importance of such partnerships within the rare diseases community. “We’re living in a time where families are playing a crucial role in leading translational research efforts beyond fundraising; it’s no longer just biotech and universities that are driving scientific progress. But we must work closely together,” he reflected. “Having that relationship with Baylor is absolutely key as we race against time to develop a therapy for UBA5 disorder.”
Dr. Heaney underscored the value of ORIP’s support for advancing research in genetic diseases and seeking answers for patients and their families. He explained that putting a name to the gene that affects a disease can be the first step in ending a patient’s diagnostic odyssey. “The vast majority of the projects that we are working on never would have happened without the funding that has been provided to us,” Dr. Heaney emphasized. “Without this funding, a lot of these questions would go unanswered—many rare diseases would not be discovered, and many patients and families might not be helped. That’s where these resources are so critically important.”
ORIP’s Precision Disease Modeling Program was established to create pipelines for cost-effective, high-throughput testing in various animal models used to study research community–nominated unique human genomic variants linked to diseases. The Centers are working to ascertain the relevance of these animal models to the molecular, cellular, pathophysiological, and/or phenotypic characteristics observed in the patient to improve the biological understanding of disease mechanisms, develop diagnostic tools, and test targeted or repurposed therapeutics. More information on the program can be found at ORIP’s website.
References
1 Pan X, Alvarez AN, Ma M, et al. Allelic strengths of encephalopathy-associated UBA5 variants correlate between in vivo and in vitro assays. eLife. 2023;12:RP89891. doi:10.7554/eLife.89891.
2 Rinaldi B, Bayat A, Zachariassen LG, et al. Gain-of-function and loss-of-function variants in GRIA3 lead to distinct neurodevelopmental phenotypes. Brain. 2024;147(5):1837–1855. doi:10.1093/brain/awad403.
3 Pan X, Tao AM, Lu S, et al. De novo variants in FRYL are associated with developmental delay, intellectual disability, and dysmorphic features. Am J Hum Genet. 2024;111(4):742–760. doi:10.1016/j.ajhg.2024.02.007.
4 Brooks D, Burke E, Lee S, et al. Heterozygous MAP3K20 variants cause ectodermal dysplasia, craniosynostosis, sensorineural hearing loss, and limb anomalies. Hum Genet. 2024;143(3):279–291. doi:10.1007/s00439-024-02657-2.
5 Harnish JM, Link N, Yamamoto S. Drosophila as a model for infectious diseases. Int J Mol Sci. 2021;22(5):2724. doi:10.3390/ijms22052724.
6 Lanza DG, Mao J, Lorenzo I, et al. An oocyte-specific Cas9-expressing mouse for germline CRISPR/Cas9–mediated genome editing. Genesis. 2024;62(2):e23589. doi:10.1002/dvg.23589.
7 Ketkar S, Burrage LC, Lee B. RNA sequencing as a diagnostic tool. JAMA. 2023;329(1):85–86. doi:10.1001/jama.2022.22843.
8 Cheng KC, Burdine RD, Dickinson ME, et al. Promoting validation and cross-phylogenetic integration in model organism research. Dis Model Mech. 2022;15(9):dmm049600. doi:10.1242/dmm.049600.



